Diagnosis & Management
Call Us
Hours
Location

Schedule An Appointment
Dry Eye Assessment and Treatment in Ken Caryl, CO
Dry eye disease is a prevalent issue where the eyes either lack adequate tear production or produce poor-quality tears. At the Eyecare Center of Ken Caryl, our expert eye doctors excel in diagnosing and managing dry eye disease, ensuring positive patient outcomes.
How tears work
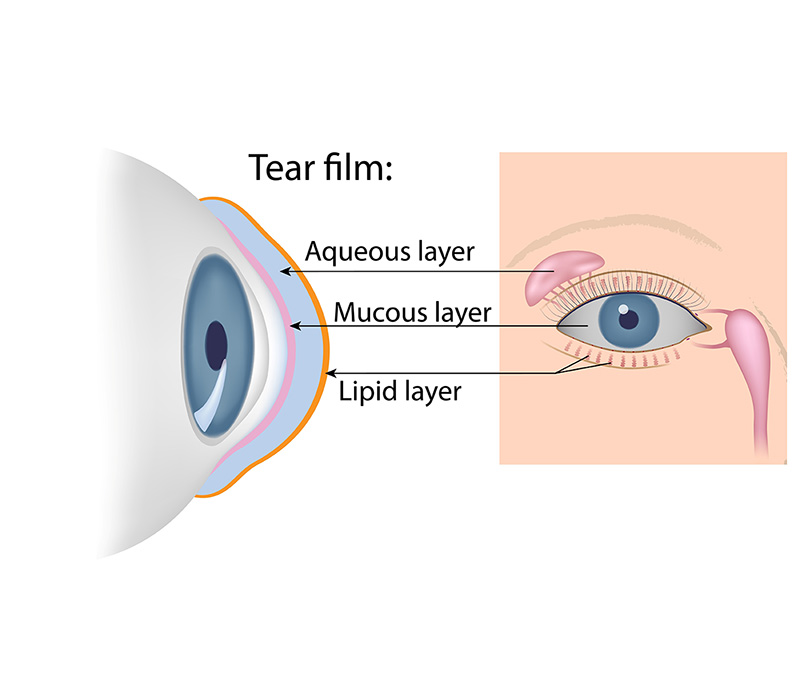
Tears play a vital role in maintaining the health and function of our eyes. They lubricate, nourish, and protect our eyes. The tear film is a complex, multi-layered structure that covers the surface of the eye. It consists of three primary layers, each with a specific function:
- Lipid (oil) layer: The lipid layer is the outermost layer and is produced by the meibomian glands located in the eyelids. This layer helps to prevent the evaporation of the watery layer beneath it, ensuring that the tear film remains stable and well-lubricated. It also contributes to the smooth optical surface of the tear film, which is crucial for clear vision.
- Aqueous (water) layer: The middle layer is the thickest of the three and is produced by the lacrimal glands located above the outer edges of the eyes. It provides hydration, lubrication, and nourishment to the cornea and the conjunctiva and helps protect the eye from infections and foreign particles.
- Mucin layer: The innermost layer is produced by goblet cells found within the conjunctiva and plays a crucial role in maintaining a stable tear film and ensuring that the eye remains well-lubricated.
The tear film’s three-layered structure ensures that the eye remains well-hydrated and maintains a smooth optical surface for clear vision.

What causes dry eye?
Numerous factors can contribute to dry eye disease. A personalized evaluation of the root causes is crucial for effective treatment.
- Meibomian gland dysfunction (MGD) occurs when meibomian glands in the eyelids become obstructed or blocked. These glands secrete an oily substance that lubricates the eye and prevents tear evaporation. Blocked glands can reduce or halt this secretion, causing tear film imbalance and dry eye symptoms. MGD is a primary cause of dry eye disease and is more common in individuals with a history of blepharitis or eyelid inflammation.
- Certain conditions, like rheumatoid arthritis, autoimmune diseases, and Sjogren’s syndrome, can cause dry eye disease.
- Some medications, such as antihistamines and antidepressants, can cause dry eyes as a side effect.
- Wind, sun, and air conditioning can also contribute to dry eyes.
- Extended screen time on computers or digital devices can lead to dry eye symptoms due to a decreased blink rate.
- Blepharitis is an inflammation of the eyelids that can cause redness, itching, burning, and grittiness. This condition can be caused by bacterial infections, overgrowth of normal eyelid bacteria, allergic reactions, or blocked oil glands, leading to dry eye disease.
- Ingredients in cosmetics like preservatives, fragrances, and certain dyes can irritate the eyes, causing dryness, redness, and itching. Eye makeup can cause irritation and dryness, especially if worn for extended periods. Cosmetics may also contribute to blepharitis by clogging oil glands, leading to bacterial overgrowth and inflammation.
- An infestation of tiny Demodex mites can cause blepharitis and dry eye disease. These mites are typically found on human skin, but large numbers on eyelashes can lead to eyelid inflammation and dry eye disease.
What are the symptoms of dry eye?
Dry eye symptoms can vary from mild to severe, including:
- Uncomfortable or painful eyes
- Burning or stinging sensations
- Itchiness
- Eye redness
- Grittiness or a sandy feeling in the eyes
- Blurry vision
- Light sensitivity
- Excessive tearing (watery eyes) can occur due to a process called reflex tearing. When your eyes are dry, it causes irritation to the ocular surface. In response, your eyes produce more tears to try to compensate for the dryness and provide relief. However, these reflex tears are usually of poor quality and don’t effectively lubricate the eye’s surface.
Untreated dry eye disease can result in more severe issues like corneal ulcers, infections, and scarring.
Dry eye disease evaluation
Our eye doctors at Eyecare Center of Ken Caryl utilize state-of-the-art diagnostic tools to assess patients for dry eye disease, identifying both the condition and its root cause.
Dry eye disease treatment
There are several treatment options for dry eye, depending on the underlying cause and severity of the condition.
Artificial tears
Over-the-counter artificial tears or lubricating eye drops can provide temporary relief for mild to moderate dry eye symptoms. They can help supplement natural tear production and improve the overall tear film quality.
Our office carries Oasis TEARS® PLUS lubricant eye drops in stock, a leading brand in dry eye relief. Oasis TEARS® PLUS are formulated to closely resemble the composition of natural tears, providing long-lasting relief from dry eye symptoms. These eye drops are preservative-free, making them gentle and safe to use for individuals with sensitive eyes.
Prescription eye drops
For more severe cases, doctors may prescribe eye drops that help increase tear production, such as Restasis, Cequa, or Xiidra. These drops work by reducing inflammation in the eye, which helps to promote tear production.
Punctal plugs
In cases where tear drainage is excessive, punctal plugs can be inserted into the tear ducts (puncta) to block drainage and help retain moisture on the eye’s surface. These plugs can be temporary or permanent, depending on the patient’s needs.
Scleral contact lenses
Scleral lenses are large-diameter, gas-permeable contact lenses that vault over the cornea and rest on the sclera (the white part of the eye). These lenses create a reservoir of fluid between the lens and the cornea, providing continuous hydration and relief from dry eye symptoms.
Environmental adjustments
Adding moisture to the air using a humidifier can help alleviate dry eye symptoms, particularly in environments with low humidity. Adjusting the environment to reduce exposure to wind, dust, or air conditioning can help minimize dry eye symptoms. Wearing wraparound sunglasses or protective eyewear can also provide relief.
Treatment for meibomian gland dysfunction
For patients with meibomian gland dysfunction (MGD) or blepharitis, gentle eyelid massages can help unblock the oil glands, improving tear film quality. Cleaning the eyelids daily with a mild cleanser can also help control inflammation and reduce symptoms.
OptiLight IPL therapy
OptiLight by Lumenis is the first and only IPL (intense pulsed light) therapy FDA-approved for the management of dry eye disease due to meibomian gland dysfunction. This innovative treatment targets the underlying causes of dry eye, providing effective and long-lasting relief.
Meibomian gland probing (MGP)
Meibomian gland probing (MGP) is a specialized procedure that targets one of the underlying causes of dry eye syndrome: meibomian gland dysfunction (MGD). MGP involves gently opening and clearing the blocked or obstructed meibomian glands, which are responsible for producing the oily component of tears. By improving the function of these glands, MGP helps restore the natural lubrication of your eyes, alleviating dry eye symptoms and enhancing overall ocular health.
Nordic Naturals supplements
At the Eyecare Center of Ken Caryl, we carry Nordic Naturals eye health supplements in stock, renowned for their high-quality formulations. These supplements are specifically designed to promote overall eye health and combat dryness by providing essential nutrients like omega-3 fatty acids, antioxidants, and vitamins. Including these supplements as part of your daily routine can contribute to the overall improvement of your dry eye symptoms.
Warm compresses
Warm compresses are a simple yet effective way to find relief from dry eye symptoms. They work by applying gentle heat to the eyelids, helping to soften and release any hardened oil in the meibomian glands. We carry warm compresses in stock at Eyecare Center of Ken Caryl, making it easy for you to access this soothing treatment at your convenience.
It’s essential to consult with an eye care professional to determine the most suitable treatment options based on the specific causes and severity of dry eye disease. Treatment plans may involve a combination of therapies for optimal results. If you are experiencing symptoms of dry eye disease, schedule an appointment at the Eyecare Center of Ken Caryl for a comprehensive eye exam. We look forward to serving you!
Can dry eye cause blurry vision?
Yes, dry eye can cause blurry vision. When your eyes don’t produce enough tears or if the tears are of poor quality, it can lead to dryness and irritation, which can then result in blurry vision. This happens because tears are essential for maintaining a smooth and clear surface on the cornea. When the cornea becomes dry or uneven due to lack of moisture, light entering the eye can scatter, causing objects to appear blurry.
Can dry eye cause headaches?
Yes, dry eye can cause headaches. When your eyes are dry and irritated, you may strain them more than usual, such as by squinting or blinking frequently to try to lubricate the eyes. This extra strain on the eye muscles can lead to headaches in some cases. Additionally, the discomfort and pain associated with dry eyes can contribute to overall discomfort that may manifest as headaches. Proper management of dry eye symptoms can help alleviate this issue and reduce the likelihood of associated headaches.
Can dry eye cause blindness?
While dry eye itself typically doesn’t cause blindness, severe and chronic cases of untreated dry eye can potentially lead to complications that may affect vision. For instance, if dry eye is left untreated for an extended period, it can cause damage to the cornea. This damage can result in corneal ulcers or abrasions, which may lead to vision problems if not addressed promptly.
However, it’s important to note that with proper diagnosis and management, including the use of artificial tears, prescription medications, lifestyle changes, and in severe cases, procedures like intense pulsed light therapy, the risk of vision loss from dry eye can be minimized significantly. Regular visits to an optometrist are crucial for monitoring and addressing any potential complications related to dry eye.
Can dry eye cause floaters?
Floaters are small, often transparent or semi-transparent specks or shapes that appear in your field of vision. Dry eye itself typically doesn’t cause floaters directly. They are caused by tiny clumps of gel or cells inside the vitreous, the gel-like substance that fills the inside of your eye.
However, if you have dry eye syndrome, you might experience symptoms like blurred vision or eye strain. These symptoms can sometimes make floaters more noticeable or bothersome, but they don’t directly cause floaters to form. If you’re experiencing an increase in floaters or other vision changes, it’s essential to consult an optometrist to rule out any underlying issues and determine the appropriate course of action.
What does dry eye look like?
Dry eye can present with various symptoms and signs, including:
- Redness: The whites of your eyes may appear red or bloodshot due to irritation caused by dryness.
- Burning or stinging sensation: You may feel a burning or stinging sensation in your eyes, especially after prolonged periods of reading, screen time, or exposure to dry or windy conditions.
- Itching: Dry eyes can be itchy, leading to a desire to rub or scratch your eyes frequently.
- Blurry vision: Vision can become temporarily blurred, especially during activities that require prolonged focus, such as reading or using a computer.
- Sensitivity to light: You may experience increased sensitivity to light due to dryness and irritation.
- Eye fatigue: Your eyes may feel tired or fatigued, especially at the end of the day or after activities that strain your eyes.
- Stringy mucus in or around the eyes: Some individuals with dry eye may notice a stringy discharge or mucus around their eyes, especially in the mornings.
- Feeling like something is in your eye: Dry eye can cause a sensation of having a foreign object or sand in your eye, leading to discomfort.
These symptoms can vary in severity and may come and go throughout the day. If you experience persistent or bothersome dry eye symptoms, it’s essential to consult with an optometrist for a proper evaluation and management plan.
Can dry eye cause eye pain?
Yes, dry eye can cause eye pain. When your eyes lack sufficient moisture, the surface of the eye becomes irritated and inflamed. This can lead to a range of uncomfortable sensations, including aching, burning, stinging, or sharp pain in and around the eyes. The pain may worsen during activities that strain the eyes, such as reading, using digital devices for extended periods, or being in dry or windy environments.
In addition to the discomfort, dry eye-related pain can also be accompanied by other symptoms like redness, sensitivity to light, blurred vision, and a feeling of dryness or grittiness in the eyes. Proper diagnosis and management of dry eye syndrome, including the use of lubricating eye drops, lifestyle modifications, and sometimes prescription medications, can help alleviate eye pain and improve overall eye comfort. Consulting with an optometrist is important to determine the underlying cause of eye pain and to receive appropriate treatment.
Can dry eye cause double vision?
Dry eye typically does not directly cause double vision. Double vision occurs when the eyes are misaligned or when there is an issue with the eye muscles or nerves that control eye movement. However, in some cases, dry eye symptoms such as blurry vision or difficulty focusing can make objects appear doubled or distorted, especially during activities that require prolonged visual concentration, such as reading or using digital screens.
Additionally, if dry eye is severe and leads to significant corneal irregularities or changes in the tear film, it may indirectly contribute to visual disturbances that can manifest as double vision. However, this is relatively rare and usually occurs in severe or chronic cases of untreated dry eye.
If you experience double vision or any other persistent visual disturbances, it’s important to consult with an optometrist for a comprehensive evaluation. They can determine the underlying cause of your symptoms and recommend appropriate treatment or referral to a specialist if needed.
Can dry eye cause eye twitching?
Yes, dry eye can contribute to eye twitching in some individuals. Eye twitching is often associated with fatigue, stress, caffeine intake, and eye strain. When your eyes are dry, they may become irritated and strained, leading to muscle spasms or twitching, particularly around the eyelids.
The connection between dry eye and eye twitching is indirect but can be significant, especially if the dry eye symptoms are chronic or severe. Addressing dry eye symptoms through proper hydration, use of lubricating eye drops, lifestyle adjustments, and possibly prescription treatments can help reduce eye strain and alleviate eye twitching in many cases.
If you’re experiencing persistent eye twitching or other eye-related concerns, it’s advisable to consult with an optometrist for a thorough evaluation and personalized recommendations. They can help determine the underlying causes of your symptoms and provide appropriate guidance for management and treatment.
Can dry eye be cured?
Dry eye syndrome is a chronic condition, which means that it typically cannot be cured completely. However, it can often be effectively managed and symptoms can be significantly reduced with appropriate treatment and lifestyle modifications.
Treatment options for dry eye may include:
- Artificial tears: Lubricating eye drops can help supplement natural tear production and alleviate dryness and discomfort.
- Prescription medications: In some cases, prescription eye drops, ointments, or oral medications may be recommended to reduce inflammation, increase tear production, or improve tear quality.
- Lifestyle adjustments: Making changes such as taking breaks during prolonged screen use, using a humidifier in dry environments, and maintaining good eye hygiene can help manage dry eye symptoms.
- Intense pulsed light therapy (IPL): This treatment can help reduce inflammation in the eyelid glands, improving tear quality and reducing dry eye symptoms.
- Nutritional supplements: Omega-3 fatty acids and other supplements may be beneficial for improving tear production and quality.
While dry eye may not have a permanent cure, ongoing management and regular monitoring by an optometrist can help control symptoms and improve eye comfort and health. It’s essential for individuals with dry eye syndrome to work closely with their optometrist to develop a personalized treatment plan that addresses their specific needs and concerns.
Can dry eye cause dizziness?
Dry eye syndrome itself typically does not directly cause dizziness. However, there can be indirect connections between certain eye conditions and dizziness. For example:
- Eye strain: Prolonged periods of focusing, especially when dealing with blurry vision or discomfort due to dry eye, can lead to eye strain. Eye strain can sometimes cause headaches, which in turn may contribute to feelings of dizziness or lightheadedness in some individuals.
- Visual disturbances: If dry eye symptoms, such as blurred vision or difficulty focusing, are severe or persistent, they can affect your ability to perceive your surroundings clearly. This can sometimes lead to a sensation of imbalance or dizziness, especially when combined with other factors such as fatigue or stress.
- Medication side effects: Some medications used to treat dry eye or related conditions may have side effects that include dizziness or lightheadedness. It’s important to discuss any medication-related concerns with your healthcare provider.
While dry eye itself is not a direct cause of dizziness, it’s essential to address any underlying factors contributing to your symptoms. If you experience persistent or concerning dizziness, it’s advisable to consult with an optometrist for a comprehensive evaluation and appropriate management.
Can dry eye cause light sensitivity?
Yes, dry eye can indeed cause light sensitivity (photophobia). When your eyes are dry and irritated, they may become more sensitive to light. This sensitivity can manifest as discomfort or pain when exposed to bright lights, sunlight, or even moderate indoor lighting.
The reason behind this light sensitivity in dry eye is related to the compromised tear film on the eye’s surface. Tears not only lubricate the eyes but also provide a protective barrier against external irritants, including light. When the tear film is inadequate or unstable due to dry eye, the eyes may become more vulnerable to light-induced discomfort.
Managing dry eye symptoms effectively, such as using lubricating eye drops, practicing good eye hygiene, wearing sunglasses outdoors, and reducing exposure to harsh environmental conditions, can help alleviate light sensitivity.
Additionally, addressing any underlying factors contributing to dry eye, such as certain medications or environmental factors, can also be beneficial in managing photophobia. If light sensitivity persists or worsens, consulting with an optometrist is recommended for a thorough evaluation and personalized treatment plan.
Can dry eye cause redness?
Yes, dry eye can cause redness in the eyes. When your eyes lack sufficient moisture, the surface of the eye can become irritated and inflamed. This inflammation can lead to dilation of blood vessels in the conjunctiva (the clear membrane covering the white part of your eye), resulting in redness or a bloodshot appearance.
Other factors that may contribute to redness in dry eye include:
- Eye rubbing: Individuals with dry eye may experience a reflexive response of rubbing their eyes to alleviate discomfort. However, this can exacerbate irritation and redness.
- Environmental factors: Dry or windy environments, as well as exposure to smoke, dust, or allergens, can further irritate the eyes and contribute to redness.
- Prolonged screen time: Staring at digital screens for extended periods without adequate breaks can lead to eye strain and redness, especially in individuals with underlying dry eye.
Managing dry eye symptoms through the use of lubricating eye drops, lifestyle adjustments, and addressing any contributing factors can help reduce redness and improve overall eye comfort. If redness persists or is accompanied by other concerning symptoms, it’s advisable to consult with an optometrist for a comprehensive evaluation and personalized treatment plan.
Can dry eye affect your vision?
Yes, dry eye can affect your vision in several ways:
- Blurry vision: Insufficient tear production or poor tear quality can lead to a lack of adequate lubrication on the eye’s surface. This can cause the vision to become blurry, particularly during activities that require prolonged visual focus, such as reading or using digital screens.
- Fluctuating vision: Dry eye symptoms can cause vision to fluctuate throughout the day. Your vision may be clearer in the morning or after using lubricating eye drops, but it may worsen as the day progresses or in dry or windy environments.
- Sensitivity to light: Dry eye can increase sensitivity to light, making it uncomfortable to be exposed to bright lights or sunlight. This sensitivity can affect your visual comfort and clarity.
- Halos or glare: In some cases, dry eye symptoms such as irregularities on the corneal surface or changes in the tear film can lead to visual disturbances like halos around lights or glare, especially at night or in low-light conditions.
- Double vision: While rare, severe dry eye or associated complications such as corneal irregularities can potentially lead to double vision (diplopia). This occurs when the eyes are unable to focus properly due to dryness-related changes in the eye’s surface.
Managing dry eye symptoms effectively through the use of lubricating eye drops, lifestyle modifications, and addressing any underlying factors can help improve vision and overall eye comfort. Regular visits to an optometrist are important for monitoring your eye health and receiving personalized treatment recommendations.
Can dry eye cause styes?
Yes, dry eye can potentially contribute to the development of styes (hordeolums). Styes are red, painful lumps that can form on the eyelid, typically near the base of the eyelashes. They are usually caused by a bacterial infection of the oil glands in the eyelids.
- Dry eye can indirectly increase the risk of developing styes through several mechanisms:
- Decreased blinking: When you have dry eye, you may blink less frequently, as blinking helps spread tears evenly across the surface of the eye. Reduced blinking can lead to stagnant tears and a higher likelihood of bacterial growth on the eyelids.
- Compromised tear film: Insufficient tear production or poor tear quality in dry eye can affect the eye’s natural defenses against bacterial infections. A compromised tear film may not effectively wash away bacteria or debris from the eyelids and eyelashes, increasing the risk of infection.
- Eye rubbing: Individuals with dry eye may experience irritation or discomfort, leading to frequent rubbing of the eyes. Rubbing can introduce bacteria from the skin or environment into the oil glands of the eyelids, potentially causing a stye.
To reduce the risk of styes associated with dry eye, it’s important to manage dry eye symptoms effectively. This may include using lubricating eye drops, practicing good eye hygiene, avoiding eye rubbing, and addressing any underlying factors contributing to dry eye. If you develop a stye or experience persistent eye discomfort, it’s advisable to consult with an optometrist for evaluation and appropriate treatment.
Can dry eye affect only one eye?
Yes, dry eye can affect only one eye, a condition known as unilateral dry eye. While dry eye commonly affects both eyes simultaneously, there are instances where one eye may experience dryness and related symptoms more prominently than the other.
Several factors can contribute to unilateral dry eye:
- Environmental factors: Exposure to dry or windy conditions, air conditioning, or heating vents can lead to localized dryness in one eye.
- Underlying conditions: Certain medical conditions or medications may affect tear production or quality differently in each eye, leading to unilateral dry eye.
- Eyelid issues: Structural abnormalities or dysfunction of the eyelids, such as meibomian gland dysfunction (MGD) or eyelid malpositions, can impact tear distribution and contribute to dryness in one eye.
- Trauma or surgery: Previous eye trauma, surgery, or injury to one eye can disrupt the normal tear film and lead to dryness.
- Allergies or infections: Conditions such as allergies or eye infections may primarily affect one eye, leading to dryness and related symptoms.
It’s important to note that unilateral dry eye should still be evaluated by an eye care professional to determine the underlying cause and appropriate treatment. Management strategies for unilateral dry eye may include using lubricating eye drops, addressing any underlying medical conditions or allergies, and practicing good eye hygiene. Regular follow-ups with an optometrist can help monitor the condition and ensure optimal eye health.
Are dry eyes itchy?
Yes, dry eyes can often be itchy. When your eyes lack sufficient moisture, they can become irritated and inflamed, leading to sensations of itchiness or scratchiness. This itching sensation is commonly experienced along with other dry eye symptoms such as:
- Burning or stinging: Dry eyes can cause a burning or stinging sensation, particularly when exposed to certain environmental factors like dry air or wind.
- Redness: Irritation from dry eyes can lead to redness in the whites of the eyes, making them appear bloodshot.
- Blurry vision: Insufficient tear production or poor tear quality can result in blurry vision, especially during activities that require prolonged visual focus.
- Sensitivity to light: Dry eyes may increase sensitivity to light, making it uncomfortable to be in brightly lit environments.
- Feeling of grittiness: Some individuals with dry eyes may experience a sensation of having a foreign object or grit in their eyes, which can contribute to the urge to rub or itch the eyes.
It’s important to avoid rubbing your eyes if they feel itchy, as this can further irritate the eyes and potentially lead to complications. Using lubricating eye drops or artificial tears can help alleviate dryness and itching by providing additional moisture to the eyes. If you experience persistent itching or other concerning symptoms related to dry eyes, it’s advisable to consult with an optometrist for evaluation and appropriate management.
Why dry eye after lasik?
Dry eye after LASIK (Laser-Assisted in Situ Keratomileusis) is a common occurrence and can be attributed to several factors:
- Temporary disruption of tear production: LASIK surgery involves creating a flap in the cornea and reshaping the underlying tissue to correct vision. This procedure can temporarily disrupt the nerves responsible for stimulating tear production, leading to decreased tear production initially after surgery.
- Changes in tear film quality: The surgical process and healing response can alter the composition and stability of the tear film, which is essential for maintaining eye lubrication and comfort.
- Reduced blink rate: Some individuals may experience a reduced blink rate or incomplete blinking after LASIK, which can contribute to evaporative dry eye. Incomplete blinking can result in inadequate spreading of tears across the ocular surface.
- Environmental factors: Factors such as dry air, wind, air conditioning, and prolonged screen use post-surgery can exacerbate dry eye symptoms.
- Pre-existing dry eye: Individuals who had dry eye before LASIK may experience a worsening of symptoms after surgery, as LASIK can further disrupt the tear film and exacerbate underlying dryness.
Managing dry eye after LASIK may involve:
- Preservative-free artificial tears: Using lubricating eye drops or artificial tears without preservatives can help alleviate dryness and maintain eye moisture.
- Medications: Prescription eye drops or ointments may be prescribed to reduce inflammation and improve tear film quality.
- Environmental modifications: Making adjustments such as using a humidifier, taking breaks from screen use, and avoiding exposure to dry or windy environments can help manage dry eye symptoms.
It’s essential to follow your optometrist’s recommendations and attend follow-up appointments after LASIK to monitor your eye health and address any post-operative dry eye symptoms effectively.